Nocturnal seizures: symptoms and treatment

Can you have a seizure in your sleep? The answer is yes, and this type of epileptic attack may happen once or be a recurring event1. Nocturnal epileptic seizures can be harder to identify and it can be difficult to distinguish from other sleep disorders such as parasomnias, which may display similar symptoms2. Just because these occur while the patient is asleep it does not mean that they are harmless. Recurring epileptic attacks lower sleep quality and cause daytime drowsiness and there is still a risk of injury while sleeping. Most nocturnal seizures will pass with little complication, but in some rare cases, nocturnal seizures can affect heart rate and breathing which can rarely raise the risk of mortality3. These are all reasons why it is important to identify nocturnal seizures and follow a quick, targeted path of treatment2. Here is how to recognise them.
Signs and symptoms of epileptic seizures in your sleep
There are different types of epilepsy each with different symptoms4. For reasons we don’t understand, seizures can happen while patients are awake or asleep - no one knows why some people are more susceptible to sleep seizures than others5. A specialist must assess each case individually, since various types of epilepsy are linked to these attacks5.
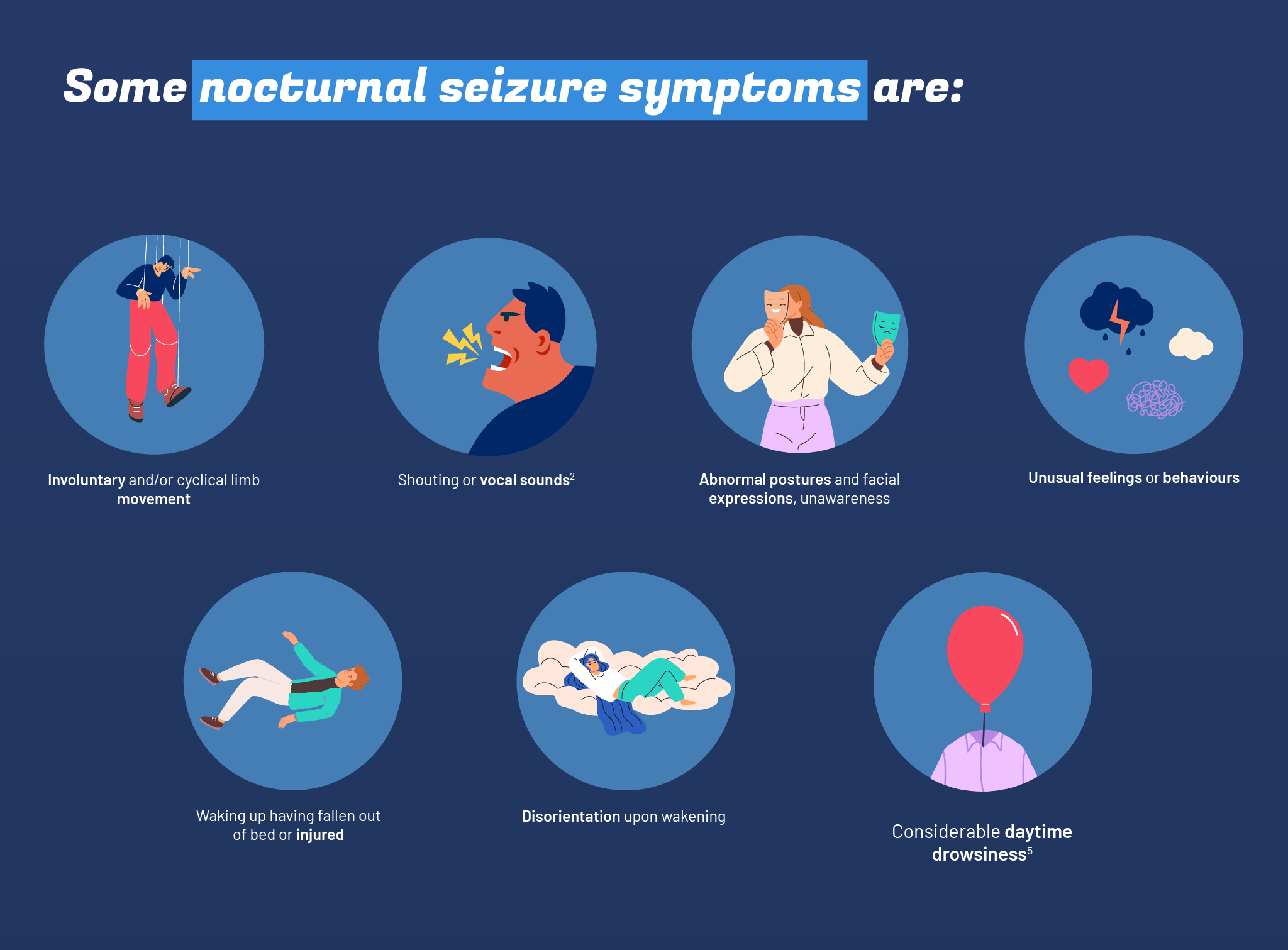
Some nocturnal seizure symptoms are:
- involuntary and/or cyclical limb movement;
- abnormal postures and facial expressions, unawareness;
- shouting or vocal sounds2;
- unusual feelings or behaviours;
- disorientation upon wakening;
- waking up having fallen out of bed or injured;
- considerable daytime drowsiness5.
Causes and diagnosis
Having an epileptic seizure does not always mean that you have epilepsy. Single seizures can be caused by some drugs or other medical conditions6, but when seizures are recurring and not brought on by a specific event – like a trauma or infection – the definition of epilepsy is fulfilled6. Epilepsy is a non-transmissible chronic disease that affects the brain which as of yet we know little about. Even today it comes with a lot of social stigma, especially on the job7,8. When the attacks mainly come at night, it might be “nocturnal epilepsy”, which includes the form of Sleep-related Hypermotor Epilepsy (SHE)3.
SHE is defined by the following characteristics:
- seizures lasting up to 2 minutes, with stereotyped movements and an abrupt start and end
- mainly hypermotor episodes, that is, with excessive involuntary movement
- epileptic seizures mainly while asleep, although daytime episodes may still occur2.
On average, patients with this type of “nocturnal epilepsy” have 8 short seizures per night9. Diagnosis is made based on medical history and specific examinations2. In addition to blood tests including any genetic testing, the primary exam is the electroencephalogram carried out while sleeping (EEG Telemetry) – a test that studies electrical activity in the brain10. Oftentimes, patients do not display any symptoms during waking hours, and if not, it might be best to do a sleep study using a polysomnography3,11, too. A CT scan and brain MRI may also provide important information12, and unusually includes a spinal tap6 (a test that withdraws and analyses cerebrospinal fluid13).
Nocturnal seizures: treatments
The treatment of nocturnal seizures is adjusted based on what is causing the attacks. If there has been a single episode with a low risk of recurrence, treatment is generally not prescribed2. Other times, the patient goes on antiseizure medications. Around 30% of patients do not respond to usual drug treatments, and surgery may be an option to assess given that it is effective in about two thirds of patients which undergo it14.
Nocturnal seizures may be helped by some simple lifestyle amendments:
- implementing proper sleep hygiene; - keep as regular a sleep pattern as possible!
- a well-balanced diet15;
- cutting or reducing the consumption of alcohol and other substances9.
Lastly, if you have symptoms suggesting nocturnal seizures, make sure you tell a doctor as soon as possible so that they can ensure that investigation and if necessary safe treatment are begun as soon as possible.

References:
- “Epilepsy Action (Uk), “After a first seizure”, October 2024
- Tinuper P., Bisulli F., Cross J. H., Hesdorffer D., Kahane P., Nobili L., Provini F., Scheffer I. E., Tassi L., Vignatelli L., Bassetti C., Cirignotta F., Derry C., Gambardella A., Guerrini R., Halasz P., Licchetta L., Mahowald M., Manni R., Marini C., Mostacci B., Naldi I., Parrino L., Picard F., Pugliatti M., Ryvlin P., Vigevano F., Zucconi M., Berkovic S., Ottman R., “Definition and diagnostic criteria of sleep-related hypermotor epilepsy”. Neurology. 2016 May 10;86(19):1834-42. doi: 10.1212/WNL.0000000000002666. Epub 2016 Apr 15. PMID: 27164717; PMCID: PMC4862248. https://pmc.ncbi.nlm.nih.gov/articles/PMC4862248/
- Sleep Foundation, “Nocturnal Nocturnal Seizures: Symptoms, Causes, Diagnosis, Treatment”, 3 May 2024
- Sarmast S. T., Abdullahi A. M., Jahan N., “Current Classification of Seizures and Epilepsies: Scope, Limitations and Recommendations for Future Action”. Cureus. 2020 Sep 20;12(9):e10549. doi: 10.7759/cureus.10549. PMID: 33101797; PMCID: PMC7575300, https://pmc.ncbi.nlm.nih.gov/articles/PMC7575300/
- “Epilepsy Action (Uk), “Sleep seizures”
- Huff J. S., Murr N. I. “Seizure”. [Updated 2023 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430765/
- World Health Organization (WHO), “Epilepsy”, 7 February 2024
- de Souza J. L., Faiola A. S., Miziara C. S. M. G., de Manreza M. L. G. “The Perceived Social Stigma of People with Epilepsy with regard to the Question of Employability”. Neurol Res Int. 2018 May 13;2018:4140508. doi: 10.1155/2018/4140508. PMID: 29862075; PMCID: PMC5971250. https://pmc.ncbi.nlm.nih.gov/articles/PMC5971250/
- Epilepsy Foundation, Joshi C., “Sleep-related Hypermotor Epilepsy (SHE)”, 19 November 2019
- Istituto Superiore di Sanità (ISS), “Epilessia – Diagnosi”, 30 January 2019
- Voderholzer U., Guilleminault C., “Polysomnography”, Chapter 31 - Sleep disorders, Editor(s): Michael J. Aminoff, FrançOis Boller, Dick F. Swaab, Handbook of Clinical Neurology, Elsevier, Volume 106, 2012, pages 527-540, ISSN 0072-9752, ISBN 9780444520029, https://doi.org/10.1016/B978-0-444-52002-9.00031-0 , https://www.sciencedirect.com/topics/psychology/polysomnography
- Epilepsy Foundation, “Tests and investigation”
- Mayo Clinic (nonprofit), Lumbar punctur (spinal tap)
- Asioli G. M., Rossi S., Bisulli F. et al., “Therapy in Sleep-Related Hypermotor Epilepsy (SHE)”. Curr Treat Options Neurol22, 1 (2020). https://doi.org/10.1007/s11940-020-0610-1
- Epilepsy Society (Uk), “Diet and nutrition”, October 2024
